Artificial heart valve
The heart valve replacement is called an artificially introduced a substitute for a natural heart valve. A distinction is made according to position ( aortic valve, mitral valve, tricuspid valve or ), by type ( mechanical and biological heart valves ) and processes ( open surgery or minimally invasive) of valve replacement.
- 3.1 surgical procedure
- 3.2 Selection of the valve prosthesis 3.2.1 Mechanical heart valves 3.2.1.1 types
- 4.1 Transcatheter Aortic Valve Implantation ( TAVI )
- 5.1 Postoperative Period
- 5.2 follow-up
- 5.3 anticoagulation
- 5.4 endocarditis
History
On September 11, 1952 Charles A. Hufnagel sat by the Georgetown University he developed a heart valve in the descending aorta of a patient one.
The first artificial heart valve with a ball prosthesis was implanted in 1961 by two Americans Albert Starr and Lowell Edwards.
In 2010, a total of 30 492 heart valve replacements were performed in Germany. The biggest share made with 26,208 ( 86.0 %) of the aortic valve. In Mitralklappenvitien was often a reconstruction possible ( 7,728 procedures), a mitral valve replacement was performed 4,146 times ( 13.6 %). The tricuspid valve played only a subordinate role with 138 procedures ( 0.4%).
Indication
The indication for surgery is made depending on clinical symptoms and objectively verifiable criteria. The aim is to facilitate the symptom, especially the prevention of acute or chronic heart failure. The following table provides a simplified overview:
Aortic stenosis
- Severe aortic stenosis and symptoms
- Severe aortic valve stenosis without symptoms with reduced pump function (EF < 50%) or pathological stress test, rapid progression
Aortic regurgitation
- Severe aortic regurgitation and symptoms
- Severe aortic regurgitation without symptoms with reduced pump function (EF < 50%) or end systolic diameter of the left ventricle > 50 mm
Mitral
- Significant symptoms and valve area <1.5 cm ² and valvuloplasty not possible
- Minor symptoms and valve area <1.0 cm ² and valvuloplasty not possible
Mitral regurgitation
- Severe mitral regurgitation and symptoms and EF > 30 %
- Severe mitral regurgitation without symptoms with EF <60 % or new-onset atrial fibrillation or systolic pulmonary arterial pressure > 50 mmHg
Open surgical technique
After indications for open surgical aortic valve replacement studies to assess the surgical and anesthetic risk are carried out. These include, for example, lung function tests and cardiac catheterization. If in the latter established coronary heart disease, in general, the system of Koronararterienbypässen is recommended, which can be done in a meeting with the valve replacement.
Surgical procedure
The operation is performed under general anesthesia, using the heart-lung machine. The thorax is opened by sawing open the sternum (medial sternotomy ). After opening of the pericardium and exposure of the heart, the heart -lung machine is connected. It allows the blood supply of the body with the elimination of the heart by clamping the great vessels. Means kardiopleger solution is brought to the heart to stop. Now, the affected heart valve is exposed. When this happens aortic valve replacement via the aorta, access to the mitral valve via the left atrium. The affected heart valve is first decalcified if necessary, and then removed. For this, the valve leaflets are excised from the valve ring. The aim is to create space for the largest possible valve prosthesis. To fix the prosthesis stay sutures are placed with Filzbewehrung. On these, the artificial heart valve is then guided and fixed in the correct position. When aortic valve replacement, the type of fixation depending on the prosthesis used is different. Biological valves without mechanical scaffold either obtain their own coronary vessels ( subkoronare technology) or, when using a larger Aortensegments used with reimplantation of the coronary arteries. Then the closure of the aorta or of the left atrium and the removal of the heart -lung machine takes place. In still beating heart then takes the closure of the pericardium and chest.
Choice of valve prosthesis
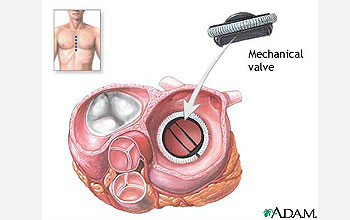
Basically, two types of prosthetic heart valves are distinguished: mechanical valves are artificially produced and consist mostly of metal, biological valves are available as transplants from human or animal.
Mechanical and biological valve prostheses differ in some respects, the basis of which the selection of patients for the most appropriate flap. Mechanical heart valves have a much longer life than biological valve prostheses. In laboratory tests, mechanical heart valves have reached a (theoretical ) Durability of 100 to 300 years. This specification refers to the expected number of opening and closing operations on the normal heart rate of 60 to 80 beats per minute. The lifetime of biological heart valves is limited, since they are subject to an accelerated aging process ( calcification ) in comparison to the native tissue. This can lead to visible and functionally significant dysfunctions that make a replacement necessary after a few years. Experience has shown that calcified biological heart valves in children earlier and faster than in adults. A significant disadvantage of mechanical valves is the coagulation activating the metal surface. This leads to an increased risk of thrombosis and thromboembolism leading to lifelong anticoagulation necessary.
Basically, mechanical valves thus be used in patients who have a high life expectancy and who have no contraindication to anticoagulation exists. Deciding which type of valve prosthesis is used, however, always based on an individual weighing all the pros and cons for each patient.
Mechanical heart valves
Mechanical heart valves are available in different designs, all of which have design-related advantages and disadvantages. Basically, there are mechanical valves of a metal body and a framework that has been provided with a polyester cuff. All mechanical designs cause a more or less audible noise dampers ( " prostheses click"). This noise is produced when closing the lid when the bounce or the flaps wings on the valve ring. The clarity of this noise is also an indication as to whether deposits have formed on the flap. All mechanical valves produce in sonography a strong reflection and an acoustic shadow.
Designs
- St. Jew -Medical: Double sliding door ( 1977 )
- Björk - Shiley: single-leaf door ( suspended discus, 1968 )
- Medtronic - Hall: single-leaf door ( discus with a central hole ). The discussion moves on a curved mandrel within the valve annulus. The valve ring is a milled titanium monoblock.
- Starr - Edwards ball cage prosthesis (first use 1952). As the valve is a plastic ball, which moves in a wire cage to the blood flow. This was the first artificial valve type and is now ( almost) irrelevant, since in this variant by the maximum design weight decisive disadvantages arise (hemolysis ).
Biological heart valves
In biological valves the valve tissue from human ( homograft ) or animal ( xenograft ) tissue is. Flaps made of artificially produced tissue ( engl. tissue engineering ) play in everyday clinical practice no significant role. The actual valve tissue is mounted on a framework ( " stent " ) or used without scaffolding. Just as artificial heart valves and biological valves for sewing are surrounded by a polyester cuff. Animal and human donor valves must be preserved after collection for later implantation. Here, the cryopreservation in liquid nitrogen has prevailed as the most effective method. Alternatives are the preparation in an antibiotic solution at 4 ° C, X-ray irradiation and Trockengefrierung.
Ross operation
A special form is the Ross operation dar. This method is used primarily in children and young adults. In the presence of a Aortenvitiums the aortic valve is removed and replaced by the patient's own pulmonary valve. The pulmonary valve can then be replaced due to the lower pressure load by a biological valve.
Minimally invasive procedures
Transcatheter Aortic Valve Implantation ( TAVI )
In addition to the open surgical technique, a catheter- based procedure in which an access path through the femoral artery ( transfemoral ) or the apex of the heart ( transapical ) is selected there. This process is called Transcatheter Aortic Valve Implantation (English transcatheter aortic valve implantation, TAVI ). The aortic valve is introduced into a metal framework. Means of a catheter is placed in the flap position. It is then unfolded and thus anchored in the valve ring. The body's own aortic valve is not removed, but replaced by the prosthesis. There are self-expanding valve distinguished from those that - are expanded using a balloon - roughly equivalent to PTCA.
The technique was first described by Alain Cribier and colleagues in 2002. The aim of TAVI is to offer the patient an aortic valve replacement, the surgical risk for open surgical replacement is overestimated. However, the minimally invasive form of therapy is so far not a general replacement for the open surgical technique. Long-term results as for Transcatheter Aortic Valve Implantation are not yet available due to the novelty of the process.
Follow-up
Postoperative Period
After surgery, the patient is first monitored at the ICU. Here also the artificial respiration is terminated. In the further course, the patient is cared for on a cardiac surgery or cardiac general ward. At the one-to two -week stay in an acute hospital closes usually several weeks of rehabilitation with controlled increasing physical stress on. A resumption of employment is possible for about ten to twelve weeks after surgery.
Follow-up
To assess the postoperative course echocardiography plays a crucial role, as the flap function ( density, pressure gradient ) and, especially in biological valves, the valve morphology can be assessed here. The first follow-up should be done after about three months.
Anticoagulation
When using a mechanical heart valve replacement lifelong anticoagulation must occur. These coumarin derivative containing medications such as warfarin, Falithrom or Phenprogamma be used. The target INR is determined by the position of the prosthesis. After biological valve replacement, anticoagulation for three months is necessary. After TAVI taking antiplatelet agents is recommended.
Endocarditis
After heart valve replacement is a lifelong endocarditis prophylaxis for all interventions in the area of the mouth and throat (eg, dental surgery, tonsillectomy ) is recommended.