Bronchiectasis
As bronchiectasis is called in medicine irreversible saccular or cylindrical extensions of the medium-sized airways (bronchi ). This condition is also referred to as bronchiectasis. These are accompanied by a widening nekrös chronic suppurative bacterial infection of the bronchial wall.
Etiology
There is an innate and an acquired form of bronchiectasis.
- Congenital bronchiectasis may occur in only one lung segment or a lobe of the lung. Also unlimited occurrences is observed, usually in conjunction with other defects ( for example, when Kartagener 's syndrome, cystic fibrosis, or nekröse and festering pneumonia ).
- Be Acquired bronchiectasis by early childhood injuries, infectious diseases ( measles, whooping cough ), allergic bronchopulmonary aspergillosis, immunoglobulin deficiency, α -1 - antitrypsin deficiency, ciliary dysfunction, cystic fibrosis, tracheoösophagale fistula, foreign body aspiration or chronic inflammation (eg chronic bronchitis).
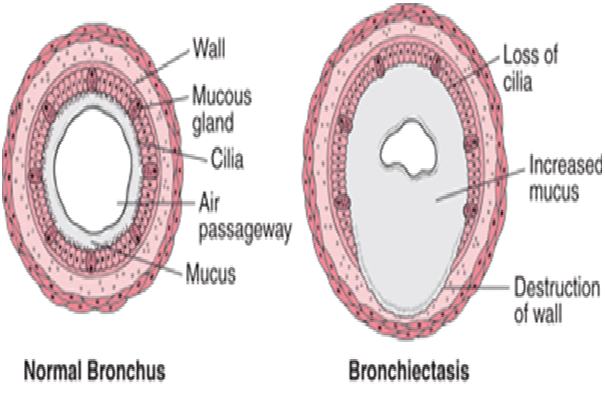
Morphology
The most significant changes occur in the lower lobes of the lungs. The bronchial expansions are
- Cylindrical
- Fusiform
- Saccular
The lumens are filled with pus.
Light microscopy shows intense accumulation of neutrophils, lymphocytes and mononuclear cells in the bronchial wall. Furthermore, to identify extensive areas of ulceration in the bronchial mucosa, this may be a squamous metaplasia in nichtgeschwürigen (epithelium ) may occur. In addition peribronchial fibrosis.
Clinic
Symptoms are cough, and large-volume discharge ( " mouth full expectoration "), and the smells sweet and insipid or foul and settles in the glass typically in three layers ( " three-tier sputum " ): foamy top layer, slimy middle class and tougher sediment with pus. Are typical finger clubbing.
Complications
Complications included pneumonia, fungal settlements in the lungs and bacterial metastases in other organs are known. Even coughing up blood ( hemoptysis ) may occur. The long term, cor pulmonale can develop. Also, a vicious circle may occur: When the bronchi are only expanded, they tend to hold back a portion of the secretions, which then serves as a nidus for persistent infection. Should an extension be perforated, this can lead to an empyema of the thorax.
Diagnosis
The disease is determined by the typical appearance and possibly by other diagnostic measures:
- Three-layer Sputum: The sputum is often frothy sero- purulent, often find themselves in the culture of Haemophilus influenzae, Streptococcus pneumoniae and Staphylococcus aureus.
- Lung function: mostly mixed restrictive - obstructive ventilation disorder and respiratory failure.
- Chest x-ray: peribronchial strip drawing and cystic cavities with or without a mirror.
- HR- CT: cystic cloudy, enlargement of the bronchial lumen; safest and most reliable bronchiectasis detection
- Bronchoscopy: for pathogen diagnostics and diagnose any Bronchusstenosen
Therapy
The focus is on physical therapy to mobilize secretions, which is also performed when symptom- free intervals exist. This includes the daily " bronchial " ( expectoration of mucus in knee - elbow position ).
Medical therapy can be considered:
- Mucolytics which thin the secretions and so facilitate expectoration
- Bronchodilator, expanding the bronchial tubes and ease breathing so
- Antibiotics in exacerbations and in severe cases, as long-term therapy ( in this case for example, prevent long-term macrolides exacerbations, but there is resistance )
- Regular immunization ( vaccination) against influenza and pneumococci.
In appropriate cases, bronchiectasis may also be removed surgically (one-sided attack, inadequate response to conservative therapy, threatening hemoptysis ).