Pancreatic cancer
Pancreatic tumors are tumors of the pancreas ( pancreatic ). If a swelling of the pancreas is found in an imaging method, it is in most cases to simple cysts or inflammation remaining pseudocysts that rarely cause symptoms need (eg a Milzvenenkompression ) and usually no treatment. However, approximately 30% of imaging studies demonstrated lesions in the pancreas are true tumors ( abnormal tissue growth ). Pancreatic tumors are classified according to the relationship to the normal tissue and the degree of malignancy ( malignancy ).
The pancreas contains exocrine gland cells whose digestive secretion accumulates in the acini and is discharged through the ducts into the duodenum, and endocrine tissue whose cells produce hormones and release into the blood. Both types of tissue can develop tumors. Therefore, pathologists distinguish exocrine and endocrine tumors. 98% of pancreatic tumors arise from the exocrine organ, namely from the ductal epithelium and acinar cells. This includes a few benign tumors ( cystadenomas and mucinous Zystome ); the rest are malignant carcinomas. Tumors of the connective and lymphoid tissue, in which the function of pancreatic tissue are embedded, are counted to the exocrine tumors. Tumors of the endocrine pancreas tissue ( islet cells ) among the neuroendocrine tumors of the gastrointestinal tract. They are subject to certain hereditary syndromes are extremely rare.
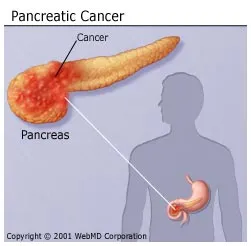
Three quarters of the tumors arise in the pancreatic head, the rightmost, located on the duodenal portion; 20 % in the central portion ( body) and five percent in the left-side foothills to the spleen out the tail of the pancreas.
- Intraductal papillary mucinous tumor - 2.1 ( IPMT )
- 2.2 mucinous cystic tumor
- 2.3 acinar cell
- 2.4 tumors of the papilla of Vater
- Serous cystadenoma 2.5
- 3.1 morphology
- 3.2 forecast
Adenocarcinoma
Adenocarcinoma (more precisely, ductal adenocarcinoma of the pancreas ) and its variants is by far the most common malignant tumor of the pancreas ( 95% of all malignant tumors of the pancreas ). The incidence is approximately 18 cases per 100,000 population per year. It thus is the third most common tumor of the digestive tract. Among the cancers in Germany pancreatic cancer is about three per cent of men in the ninth, the seventh in women. Among the cancer deaths, it is because of its high mortality ( mortality ) in Europe depending on the country even the seat 4-7 ( Germany: 4th place).
Causes
The etiology of ductal adenocarcinoma is unclear, but as a high risk of disease, chronic pancreatitis are (mostly by long-term alcohol consumption), obesity, smoking, diabetes mellitus, cystic changes (tumors) and chemical carcinogens ( naphthylamine, benzidine, nitrosamines ). By means of genetic testing, changes of the K- ras gene (mutation at codon 12) on chromosome 9 locus, as well as p21, the p53 gene on chromosome 17 q are detected in a majority of tumors. Also, polychlorinated biphenyls ( PCBs), for example, contain as plasticizers in paints and adhesives, benzene compounds, or some pesticides such as DDT increase the risk of developing pancreatic cancer and are therefore involved as causative factor under suspicion. Similarly, the development of a pancreatic tumor to genetic causes can be traced. Thus, the risk of disease increased by 20 - to 60-fold, when two or more first-degree relatives are also affected.
Pathology
The tumor occurs preferentially on (60 to 70%) in the pancreatic head and is at diagnosis, usually two to five centimeters ( detectable by imaging from about one centimeter size). He is ill-defined, firm consistency and gray - yellowish color. CT scan of the tumor in the arterial phase is demarcated hypodense. It often leads to a narrowing of the flow through the pancreas route of the bile duct, often to a stenosis of the pancreatic ductal. The tumor may grow into the wall of the duodenum, continues also important vascular structures such as the superior mesenteric artery, the splenic vein, the vena porta and / or the inferior vena cava infiltrate. The finding of these investments are for the staging and thus for the further therapeutic procedure of the utmost importance.
The histological picture is characterized by atypical, often relatively well-differentiated vein-like glandular structures with mucus production. The main histological variants of ductal adenocarcinoma are the adenosquamous carcinoma, mucinous carcinoma nichtzystische and anaplastic (undifferentiated ) carcinoma.
The first metastases are found in the adjacent lymph nodes and - via the blood stream of the portal vein - in the liver. Tumors in the pancreas body and tail of the pancreas are at diagnosis in most cases greater than the pancreatic head tumors and usually have already led to liver metastases or peritoneal carcinomatosis (infiltration of the peritoneum ).
Symptoms
The main symptom of pancreatic head carcinoma is the steadily increasing painless (that is not accompanied by colic ) icterus ( jaundice), which is caused by the narrowing of the bile duct. However, in contrast to carcinoma in the major duodenal papilla ( the mouth of the bile duct ) of jaundice is not a prodrome. More common, but uncharacteristic symptoms include weight loss and abdominal pain radiating to the back. The closure of the pancreatic duct leads to inflammation that affects the glands function and can lead to digestive problems, weight loss and diabetes.
Diagnostics
The tumors can be detected by ultrasound, endoscopic ultrasound, magnetic resonance imaging and computed tomography. The closure of the biliary or pancreatic duct is the main criterion in the ERCP. The tumors usually produce the tumor marker CA 19-9 and to some extent the non-specific CEA, which can be detected in the serum in increased concentration.
The TNM classification is used for uniform international classification of extent of malignant tumors. When pancreatic cancer it is carried out as follows:
Therapy
- The curative surgery ( surgery in healing intention ) is often made impossible by the spread of the tumor and the surrounding wall of the adjacent blood vessels. Localized tumors can be surgically removed. If the tumor is detected early and confined to the pancreas, the patient by a partial removal of the pancreas ( pancreatectomy ) can be cured. In about 80 % of patients, however, this is not true. Exemplary illustration of a partial removal of the pancreas
- Palliative operations are used for symptom relief: for example, a connection between the congested bile duct and the intestine with the Choledochojejunostomy created to divert the bile from the liver.
- ERCP may also be used for ameliorating treatment except for the diagnosis by providing a stent ( supporting tubes) is inserted into the bile duct. The jammed bile duct is made passable again by the stent.
- Not resectable ( non-removable ) tumors may be treated with chemotherapy, such as gemcitabine.
In order to improve care and to be fairly recent findings, the German Society of Gastroenterology, Digestive and Metabolic Diseases ( DGVS ) in December 2013 has issued an updated S3 guideline " Exocrine pancreatic cancer ." In this, the focus is mainly on the palliative therapy because the tumor is often too advanced to be successfully operated can. But the surgical and neoadjuvant and adjuvant chemotherapy are discussed in detail. The German Cancer Aid has funded the guideline and it was first published in collaboration with the German Cancer Society as a free booklet with the goal of nationwide to ensure an equivalent care of patients with pancreatic cancer according to latest research.
Course and prognosis
The biliary obstruction leads to hepatic dysfunction. The local tumor spread may also have a duodenal stenosis ( narrowing of the duodenum ) and ascites (abdominal fluid ) in peritoneal result. Sometimes a thrombophlebitis.
The prognosis of pancreatic cancer is poor. Only 10 to 15 % of the tumors at the time of diagnosis still operable. Recent studies show that the five- year survival rate after such a carried out in curative intent engagement between three and 25 percent. Inoperable tumors also speak poorly to chemotherapy.
Exocrine pancreatic tumors
Among the tumors of the exocrine pancreas:
Intraductal papillary mucinous tumor - ( IPMT )
Synonym: intraductal papillary mucinous carcinoma -. These tumors are characterized by the formation and propagation within the duct system. They usually grow in the pancreatic duct in the head of the gland. We distinguish a main course type, a Seitenasttyp and a combined type. The normal ductal epithelium is replaced by high cylindrical neoplastic cells in small nodular - wart-like ( papillenförmigen ) growths that form viscous mucus. The latter flows from difficult. This leads to irregular extension of the transition section affected three to four inches. The tumor cells can also spread to the side passages and grasp the entire pancreas in a rare case. Approximately 30 % of patients already exist vessel dips and so invasive cancer, then mostly as mucinous carcinoma nichtzystisches ( colloid carcinoma) referred because of mucus lakes in the parenchyma of the organ.
The intraductal papillary mucinous tumors occur in men slightly more frequently than in women and occur primarily between 60 and 70 years of age. Common symptoms include pain and pankreatitisartige after a long illness duration exocrine pancreatic insufficiency (failure of digestive enzymes). The cause of these symptoms are caused by the tumor tissue and mucus obstruction of the pancreatic duct, which results in that the pancreatic tissue scarring as chronic obstructive inflammation ( pancreatitis).
The prognosis of intraductal papillary mucinous tumors is very good if the tumor can be completely removed. This also applies to the invasive carcinoma, when the cancer has not yet exceeded the pancreas.
Mucinous cystic tumor
Synonym: mucinous cystadenoma, cystadenocarcinoma. ( Gross cystic ) cystadenomas have a tendency to degeneration cystadenocarcinoma. Imaging technique can not differentiate be made, so benign and malignant variants are summarized under the term mucinous cystic tumor. Women between 40 and 60 years of age are preferentially affected. The tumors have a broad fibrous capsule and hold about two to twelve inches in diameter. They consist in the vast number of less than six cysts with a single diameter of about two centimeters. These cysts are lined with epithelium and muzinproduzierendem either differentiated good or show significant atypia. Laboratory tests covered a rise in carcinoembryonic antigen ( CEA), as well as in the majority even of CA 19-9 on. If we succeed in total resection of the tumor, the prognosis is good. In malignancies, the five- year survival rate is about 75 %
Acinar cell
This rare tumor of the acinar cells is twice as common in men as in women ( peak age 55 to 65 years). Although the tumors are usually relatively large ( 4-6 cm), they are often not detected until they have already metastasized to the liver. On occasion, Azinuszellkarzinomen due to a massive secretion of lipases from the tumor cells to subcutaneous Fettgewebenekrosen and polyarthralgia.
Tumors of the papilla of Vater
The tumors of the papilla of Vater ( duodenal papilla major, mouth of the bile duct ) are mostly adenocarcinomas as well as the ductal pancreatic cancers. Occasionally these cancers go forth from tubulovillous adenomas that correspond histologically adenomas of the duodenum. The prognosis of Papillenkarzinoms is better than that of pancreatic cancer, since the rapidly occurring jaundice leads to early diagnosis of the tumor. Spread and metastasis run like pancreatic.
Serous cystadenoma
Synonym: microcystic ( cyst ) adenoma. This benign tumor is observed predominantly ( 3:2 to 9:2 ) in women of advanced age and represents 10 to 30% of a random finding dar. It is more common in the pancreatic head, but each region may be affected. He can to about six to ten centimeters in size and consists of small cysts with serous contents, which are often divided by delicate septa. In addition to a central scar can be found in more than one third of cases central calcifications. The cysts are lined with cuboidal epithelium, histologically, there are no atypia or mitotic figures. Serous cystadenocarcinomas are rare. An association with the von Hippel -Lindau syndrome has been described, the tumor may eat a large sections of the pancreas. Laboratory tests, the CEA is negative. The tumor has no degeneracy trend and has a good prognosis after resection.
Endocrine tumors
Among the tumors of the endocrine pancreas:
- Insulinoma
- Gastrinoma ( Zollinger -Ellison syndrome)
- Somatostatinoma
- Glucagonoma
- VIPoma ( Verner - Morrison syndrome)
These are tumors with histologically endocrine structure ( " islet cell tumors "). By the uncontrolled secretion of hormones (insulin, gastrin, vasoactive intestinal peptide or glucagon ) characteristic syndromes may be caused. In this case, the tumors are therefore classified as insulinomas, gastrinomas, and VIPomas glucagonomas. Suction. other hand, non-functional tumors have no hormonal symptoms.
Endocrine pancreatic tumors make up only one to two percent of all pancreatic tumors and can occur at any age. A clustering of cases can be found in the syndrome of multiple endocrine neoplasia ( MEN1 syndrome). Otherwise neuroendocrine pancreatic tumors in childhood are extremely rare; in adults, they occur in all age groups and in both men and women about equally common, but are of very often. The prevalence is below 1 / 100,000. Insulinomas and gastrinomas make 60 %, non- functional tumors 30 % of these neoplasms from.
Morphology
It is well-defined, round solitary tumors with a diameter of one to four centimeters that can occur in all parts of the pancreas. Histologically, it is monomorphic tumor cells with a feingranulären cytoplasm. The cells are arranged in solid, trabecular and pseudoglandulär. The immunocytochemical presentation of hormones allows a functional - morphological classification of these tumors. Electron microscopy can be found in the tumor cells membrane-bounded neurosecretory Hormongranula. It can be found monomorphic cells with round nuclei. Immunohistology are endocrine tumors positive for the marker CGa, Syn and NSE.
Although the neuroendocrine pancreatic tumors are highly differentiated histologically, they behave with the exception of insulinoma often malignant. This is especially true for gastrinomas, VIPomas, glucagonomas and nonfunctional tumors. Since the histological criteria of malignancy of these tumors are unreliable, only the presence of metastasis, or tumor invasion into surrounding bodies can ensure the detection of the malignancy. The first metastases are found in the regional lymph nodes and liver. Despite metastasis often long survival times ( five to ten years) can be observed.
Forecast
The prognosis for benign ( benign ) tumors is good. Malignant ( malignant ) forms, the mean survival time ½ year, wherein individual patterns are described more than two years.
Criteria to assess the prognosis of pancreatic endocrine tumors (WHO 2000)
- A infiltration of adjacent organs (eg, duodenum, stomach)
- B insulinomas
- C insulinomas and other functionally active tumors (e.g., glucagonomas )
In addition, there are hormoninaktive ( neuro) endocrine tumors of the pancreas, which can form small amounts of hormones though, but do not release and therefore no symptoms iS of hormonal overproduction cause ( such as the above-mentioned gastrinomas, insulinomas, etc.). You can remain asymptomatic for a long time.
A relatively reliable tumor marker for neuroendocrine tumors ( endocrine disrupters and hormone inactive ) is chromogranin A ( CgA ), which can be determined in the blood. In 60-80 % of all patients shows an increase of CgA.
Statistical information
In Germany the disease in about 15,400 people on pancreatic cancer. The average age of onset for men is 68 years, whereas women at 75 years.